(Posterior Vitreous Detachment)
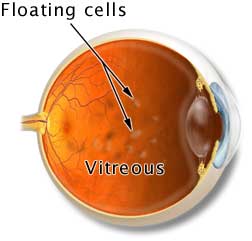
The space between the crystalline lens and the retina is filled with a clear, gel-like substance called vitreous. In a newborn, the vitreous has an egg-white consistency and is firmly attached to the retina. With age, the vitreous thins and may separate from the back of the eye. This is called posterior vitreous detachment (PVD), a very common, usually harmless condition.
As the vitreous pulls free from the retina, it is often accompanied by light flashes or floaters. Floaters are caused by tiny bits of vitreous gel or cells that cast shadows on the retina. Flashes occur when the vitreous tugs on the sensitive retinal tissue.
There are other more serious causes of flashes and floaters, however. Retinal tears, retinal detachment, infection, inflammation, haemorrhage, or an injury such as a blow to the head may also cause floaters and flashes. (Have you ever seen stars after bumping your head?) Occasionally, flashes of light are caused by neurological problems such as a migraine headache. When related to a headache, the flashes of light are seen in both eyes and usually lasts 20-30 minutes before the headache starts.
Signs and Symptoms
- Black spots or "spider webs" that seem to float in the vision in a cluster or alone
- Spots that move or remain suspended in one place
- Flickering or flashing lights that are most prominent when looking at a bright background like a clear, blue sky
Symptoms that may indicate a more serious problem
- Sudden decrease of vision along with flashes and floaters
- Veil or curtain that obstructs part or all of the vision
- Sudden increase in the number of floaters
Detection and Diagnosis
Notify your eye care practitioner immediately if you notice a sudden shower of floaters, new light flashes, a veil or curtain obstructing your vision, or any other change. The eye care practitioner will dilate your pupils with drops and examine the vitreous and retina inside the eye with an ophthalmoscope.
Treatment
Because of the risk, surgery is rarely indicated for PVD except when the floaters obscure the vision. In these cases, surgical removal of the vitreous (vitrectomy) may be considered only if the vision is significantly affected. This treatment is rarely needed since floaters typically become less bothersome over a period of weeks to months as they settle below the line of sight.
If the flashes and floaters are related to a problem other than a PVD, surgical treatment may be required.
Be proactive and monitor your vision
It is important to periodically assess the vision of each eye. Many problems can be detected early by simply comparing both eyes.
To test your vision:
- Cover one eye and pick a point to look at straight ahead
- Note the quality of your central and peripheral vision, noting any change
- Look for any obstructions, veils or curtains in your peripheral vision
- Watch for floaters, flashes
- Note the duration and intensity of the symptoms
- Cover fellow eye and repeat
Report any new symptoms or changes in vision to your eye care practitioner.
Illustrations by Mark Erickson
With acknowledgement to St. Lukes Eye Hospital.
